If you’re reading this, chances are you’ve noticed your joints move a little (or a lot!) more than others. Maybe you have pain or other unexplained symptoms that seem random. Maybe you can touch your thumb to your forearm, or perhaps your knees hyperextend when you stand. Maybe you saw a video of someone doing these things that has now led you down a rabbit hole of online research, bringing you to terms like “Ehlers-Danlos Syndrome” (EDS) or “Hypermobility Spectrum Disorder” (HSD).
It can feel overwhelming, and others have been where you are too! Many people live with hypermobility, and understanding whether it’s part of a broader condition like EDS or HSD is the first step toward managing your symptoms and improving your quality of life.
What’s the Difference Between Hypermobility, HSD, and EDS?
Hypermobility
This just means your joints have a greater range of motion than average. Think of it like a spectrum. Some people are naturally more flexible. For many, this is just a cool party trick and doesn’t cause any problems.
Hypermobility Spectrum Disorder (HSD)
If you have hypermobility and you’re experiencing pain or other symptoms because of that hypermobility, but you don’t fully meet the criteria for a specific EDS type, you might be diagnosed with HSD.
HSD is like having a collection of hypermobility-related issues that significantly impact your life.
Hypermobile Ehlers-Danlos Syndrome (hEDS)
This is a specific genetic connective tissue disorder. While hypermobility is a key feature, hEDS involves a broader range of systemic symptoms beyond just the joints.
hEDS is often diagnosed based on a detailed set of criteria that look at your joint laxity, skin characteristics, and other related issues that show how widespread the connective tissue difference is throughout your body.
Other Types of Ehlers-Danlos Syndrome
There are actually currently 13 known types of EDS! The most common one is hEDS described above and that’s the only one without a currently identified single genetic mutation (they’re working on identifying groups of genetic mutations that lead to this type, so stay tuned!). However, the other 12 identified types all have genetic mutations associated with them that require comprehensive genetic testing to diagnose. You and your doctor will determine based on personal and family medical history whether genetic testing is warranted to see if you have one of the more rare types.
It’s important to remember that EDS and HSD are both legitimate conditions that can cause significant challenges. The main difference lies in the specific criteria met during diagnosis. Both benefit from similar management strategies!
So, How Do Doctors Figure This Out?
There isn’t one single “hypermobility test.” Diagnosis usually involves a few key steps:
Detailed Medical History
Your doctor will ask you a lot of questions about your symptoms, when they started, how they affect you, and if there’s a family history of similar issues. They might ask about things like frequent sprains, easy bruising, digestive problems, or even issues with your heart rate.
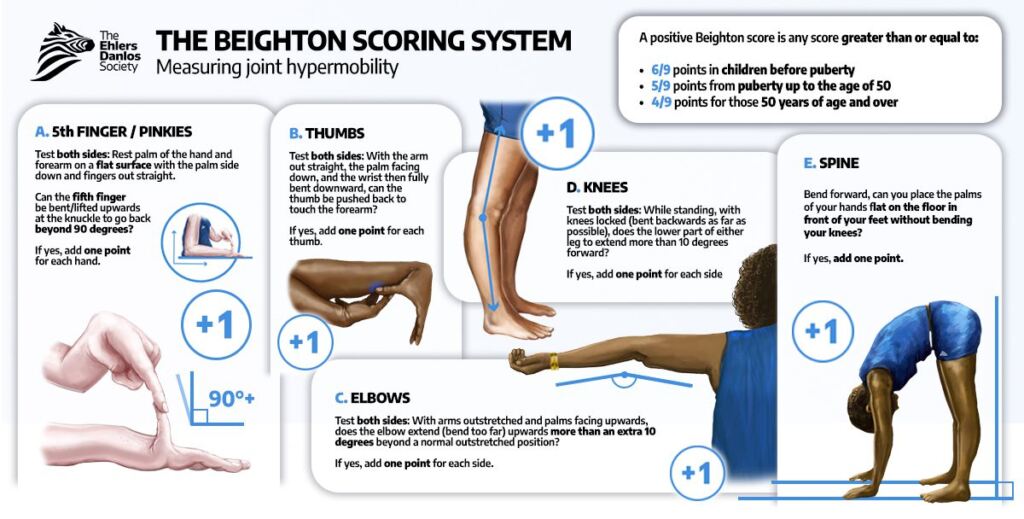
The Beighton Score
This is a simple, quick way to assess joint hypermobility. It involves checking the flexibility of specific joints like your pinky fingers, thumbs, elbows, and knees, and seeing if you can touch the floor with straight legs. It gives a score out of 9. Here’s what some of these movements look like:
Evaluating Other Criteria (for hEDS)
For a hEDS diagnosis, doctors also look for other “systemic” signs related to connective tissue weakness. These can include:
- Skin characteristics (soft, stretchy, easily bruised)
- Specific types of scarring (like “atrophic” or “papyraceous” scars)
- Pelvic organ prolapse, hernias, or rectal prolapse
- Dental crowding or a high, narrow palate
- Mitral valve prolapse in the heart
Exclusion of Other Conditions
Sometimes, other conditions can mimic hypermobility symptoms, so your doctor will want to rule those out.
Diagnosis can take time and often involves specialists. Don’t get discouraged if it’s not a quick process!

How Can Specialized Physical Therapy Help?
This is where the magic happens! While you can’t “cure” hypermobility, you can absolutely learn to manage it and reduce your pain and other symptoms. This is precisely what specialized physical therapy for hypermobility aims to do.
Think about it: if your joints are extra flexible, the muscles surrounding them have to work extra hard to provide stability. If those muscles aren’t strong and coordinated, your joints can move into uncomfortable or even damaging positions, leading to pain, dislocations, or subluxations (partial dislocations).
This is what leads a lot of patients to be afraid of movement, so it’s super important to partner with an experienced physical therapist to help guide you on how to safely trust your body to do its job!
Here’s how a PT experienced in hypermobility can help:
Strengthening
Stronger muscles create a “brace” around your joints, providing stability where your connective tissue might be lacking.
Clinical research provides compelling evidence that strengthening is not only safe but essential for EDS management. Studies have reported improvements in joint stability and body pain following strengthening and stability exercises [1].
More excitingly, heavy resistance training has been shown to be feasible and effective, even in patients with Classical EDS (cEDS), indicating that both tendon and skeletal muscle properties can be improved through resistance training [2]. How cool is that??
The physical therapist must create a tailored strengthening program that accounts for individual limitations, focusing on starting with low-impact exercises, proper technique, and gradual progression. Expertise is paramount in teaching techniques that protect the hypermobile joints, such as precise body mechanics and alignment.
Start low and slow, focusing on time under tension, while gradually increasing the muscles’ capacity for load!
Manual Therapy
To facilitate the transition to effective movement, you must also address the chronic muscle tension that frequently arises because the muscles are forced into constant compensatory work due to inherent joint instability [3].
Specialized techniques, such as dry needling, gentle mobilizations, and soft tissue work are principles of management aimed at relieving pain where possible [1]. These preparatory techniques are critical because they unlock the patient’s capacity to engage in strengthening exercises without the interference of inhibitory muscle pain.
Think of your muscles as the engine of a car. If you have a muscle that’s very tight, it’s like driving with the emergency brake slightly engaged.
When you try to press the gas pedal (strength training), the muscle struggles, and all your effort is wasted fighting that brake.
Manual therapy (like gentle massage or dry needling) is the PT carefully releasing the emergency brake. We have to let the muscle move freely first before we can effectively load it!
Patient Education
Hypermobile patients frequently experience persistent nociceptive input due to a faulty proprioceptive system, which can trigger central sensitization in the dorsal horn neurons [4].
Woah, okay I just lost 99% of you… bringing me to my exact point of why patient education matters!
This crazy sentence I threw at you is a fancy way of saying the nervous system is getting overwhelmed with signals from the body as a type of alarm security system telling it something is wrong.
This is usually due to changes in the sensitivity of that alarm system over time.
Another analogy: The nervous system changes I’m talking about are like if the smoke detector in your house were to go off when you light a candle. It’s detecting the right thing, just not at the right level. Simple, everyday stimuli can cause a disproportionate surge of pain that feels overwhelming.
Pain education itself functions as a form of desensitization therapy. By explaining that pain is an output (an overreaction by the hypersensitive nervous system) rather than an input (direct, continuous tissue damage from the movement itself), you can better understand what’s happening in your body.
It’s your physical therapist’s job to provide clear, non-jargon educational material that helps you understand the fundamental biological mechanisms driving your symptoms.
This process of education reduces fear and fosters self-efficacy. But also opens the door for you to learn more about pain science and understand how cool that thing about the dorsal horn neurons is!
Addressing Co-Morbidities
Patients with hypermobility tend to have other conditions as well, such as Postural Orthostatic Tachycardia Syndrome (POTS).
Head over to my blog post about PT for POTS to read more about how physical therapy can help manage these symptoms and how EDS-aware PTs can modify treatment in the presence of POTS!

Okay, I Know More About Hypermobility… Now What?
Since hypermobility requires a specialized approach, it’s crucial to find a physical therapist who understands the nuances of EDS and HSD.
An untrained PT might mistakenly try to stretch you (often counterproductive when you are already hypermobile) or give you exercises that unintentionally cause injury.
A physical therapist is likely a right fit for you if they…
Promote Specialized Training
They mention experience with Ehlers-Danlos Syndrome (EDS), Hypermobility Spectrum Disorder (HSD), chronic pain, vestibular issues, or pelvic floor dysfunction (all common co-occurring issues).
Focus on Stability
They emphasize exercises that promote stability, control, and muscle endurance, not just muscle bulk or the equally scary opposite of never touching weights!
Use a Manual Therapy Approach
They use gentle manual therapy (like the “emergency brake release” we talked about!) to ease tight, overworking muscles before starting strength work.
Have a Holistic View
They ask questions about things beyond your joints, such as fatigue, heart rate changes, digestion, or sleep, recognizing that hypermobility is a systemic issue.
Don’t be afraid to call their office and ask directly:
“Do you have experience working with patients who have hypermobile Ehlers-Danlos Syndrome or Hypermobility Spectrum Disorder?”
What to Bring to Your First PT Session
You wouldn’t go to a mechanic without telling them what’s wrong with the car! Prepare for your first PT visit to make the most of your time by bringing:
Your “Pain Map”
Make a list or draw a simple diagram showing your PT exactly where and when you experience pain, instability, or “clicky” joints.
Your Diagnosis (If Applicable)
Bring any relevant documents, such as your Beighton Score, diagnosis letters, and notes on any previous injuries.
Your Medication and Symptom List
Note any medications, supplements, and related conditions you have (like POTS, MCAS, etc.). These pieces of information help them understand the full scope of your connective tissue issues.
Your Comfy Clothes
Wear clothing that allows you to move and for the PT to easily examine you. Most people wear (or bring) shorts and a workout top or t-shirt.
Your Goals
What do you want to be able to do? Walk around the block with your dog? Lift your cat when they’re puking on your favorite rug? Cook dinner without pain? Stand to take a shower?
Having clear goals gives your PT a target to work toward.
The Takeaway
Receiving a diagnosis of HSD, EDS, or hEDS can be validating, scary, and overwhelming all at once. And that’s okay!
Remember this: the key to living well with hypermobility is stability and control, not shying away or letting it control you.
You’re the boss (!) and working with a specialized physical therapist provides you with the tools to build the muscular support your flexible joints need.
Be patient with your body, celebrate the small victories, and remember that you are taking a crucial step toward better health!
Sources
- Physical therapy for hypermobility – The Ehlers-Danlos Support UK, https://www.ehlers-danlos.org/information/physical-therapy-for-hypermobility/
- Functional adaptation of tendon and skeletal muscle to resistance training in three patients with genetically verified classic Ehlers Danlos Syndrome – PMC, accessed November 20, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4241422/
- Physical Therapy – The Ehlers Danlos Society, accessed November 20, 2025, https://www.ehlers-danlos.com/physical-therapy/
- Central sensitization as the mechanism underlying pain in joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type – PubMed, accessed November 20, 2025, https://pubmed.ncbi.nlm.nih.gov/26919608/
About the Author
Dr. Morgan Groover is a physical therapist based in Chantilly, VA. She treats pelvic health, orthopedic conditions, post-operative care, active adults and athletes, individuals with hypermobility, and people with POTS. As a former swimmer and current practitioner of an active lifestyle herself, Dr. Morgan Groover is ready to help you move better, live well, and get back to doing what you love.








