Pain vs. Discomfort: Navigating the Athletic Landscape
As an athlete, understanding the difference between pain and discomfort is crucial for optimal performance and recovery. While both can be unpleasant sensations, they require distinct approaches within physical therapy.
It’s important to note that chronic pain and discomfort can lead to athlete burnout, a condition characterized by emotional exhaustion, physical fatigue, and decreased motivation. Studies have shown that a significant percentage of athletes experience burnout due to injuries and the psychological challenges/stresses associated with them (2). By effectively managing pain and discomfort, athletes can reduce their risk of burnout and maintain their overall well-being.
This blog post will explore the nuances between pain and discomfort, discuss the role of RPE (Rate of Perceived Exertion) in managing these sensations, and provide strategies for effective stress control.
Pain vs. Discomfort: A Crucial Distinction
Pain is a complex sensation that often signals underlying tissue damage or injury. It’s a protective mechanism that warns the body of potential harm. Discomfort, on the other hand, is a milder sensation that may arise from overuse, fatigue, or other factors. The key differences between pain and discomfort can be categorized between intensity, cause, and response. Below is a table to easily compare the 2 confused sensations.
| PAIN | DISCOMFORT | |
| Intensity | Typically an intense/sharp sensation, may be accompanied by other symptoms like swelling or redness, and can interfere with daily activities | Usually less severe, often related to tightness, stiffness, or soreness sensations. |
| Cause | Stems from actual or perceived tissue damage or irritation resulting from injury, illness, medical procedure, or chronic conditions | Caused by various factors, including fatigue, overuse, extended poor posture, stress, and poor sleep quality |
| Response | Requires rest and physical therapy interventions to promote healing | Managed with self-care strategies like stretching/active mobility activities, rest, hydration, and/or lifestyle changes |
It is important to note that prolonged discomfort can eventually lead to tissue damage and become a painful experience. So be aware to catch those discomfort signals before it’s too late! If you’re experiencing persistent pain or discomfort, consult with a healthcare professional for proper evaluation and treatment.
The Role of RPE in Pain Management
We love scales and measuring tools in physical therapy, but this one may be my favorite.
RPE is a subjective measure used in physical therapy to gauge exercise intensity. It’s particularly helpful for tailoring treatment to specific conditions, such as chronic pain, neurological disorders, and cardiac rehab.
As research progresses and continues to provide the rehab field more exercise/training recommendations, RPE helps us identify the most beneficial exercises for each patient, especially athletes seeking to avoid injury and manage discomfort.
RPE Explained
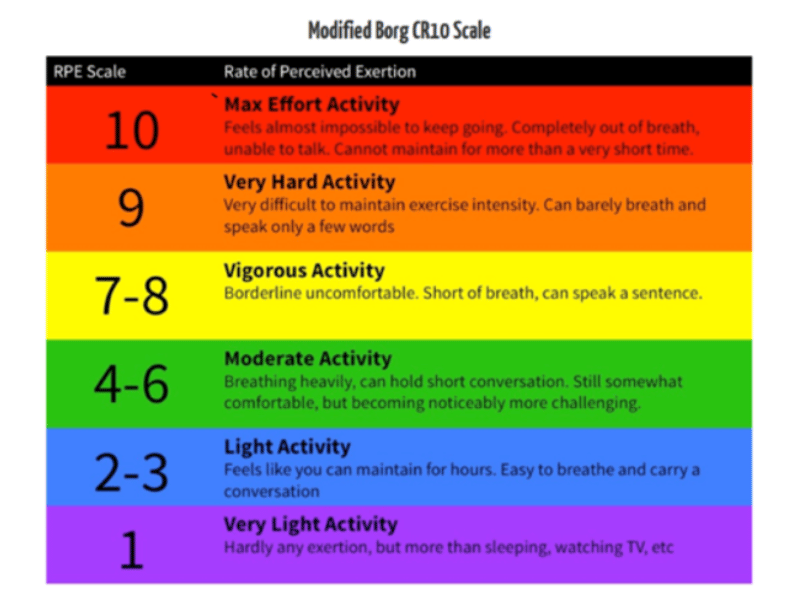
There are multiple interpretations of the scale now, but most rehab facilities utilize the modified Borg scale, which ranges from 0 to 10, with 0 representing no exertion and 10 indicating maximal effort as shown in the image above.
When engaging in a physical activity, you assess your perceived level of exertion based on factors like heart rate, breathing, muscle fatigue, or overall sensation you experience with the exercise.
Pain Threshold
Athletes should identify their pain threshold, the point at which discomfort becomes unbearable. For most athletes, an RPE of 1-3 is “discomfort” and an RPE >5 is considered “pain”.
By staying below their pain threshold, athletes can effectively manage discomfort and prevent further injury while also experiencing strength gains.
Training adjustments
Exercises are typically considered “safe” or therapeutic in sub-max or moderate exercise intensities (4-6/10 on RPE scale) with no other concerning sensations such as instability, weakness, or swelling.
As the scale demonstrates, higher perceived exertion is associated with greater exercise intensity, but there’s ongoing debate about how closely RPE aligns with the percentage of one-repetition maximum (1).
Please know this changes when you are no longer experiencing pain or discomfort – training with the RPE scale when healthy leads to a very different interpretation than what I am discussing in this blog post currently.
What if I’m starting my session with pain over 5/10?
Though not ideal, this is a very common occurrence in physical therapy. If you are comfortable to perform exercises prescribed to you by your physical therapist, typically 2 pain level increases are allowed.
Your therapist may modify sets/reps/resistance to allow execution of your exercise safely, but we know movement is needed to encourage healing, so you need to have a good rapport between yourself and your therapist to properly communicate this!
Stress and Recovery: Shifting from Threat to Challenge
Given the significant impact of pain and discomfort on athlete performance and well-being, effective stress management strategies are crucial. As we’ve discussed, the RPE scale can be a valuable tool for monitoring exertion and preventing burnout. However, managing the psychological and emotional aspects of pain is equally important.
The stress of managing pain can be compounded by its impact on sports or activities, leading to mood swings and a lower quality of life. This can create a vicious cycle, exacerbating pain and hindering recovery.
Let’s delve deeper into how athletes can cultivate a healthier relationship with stress to optimize their recovery and performance.
To truly understand how to implement effective stress management strategies, you need to understand what exactly “stress” is to each individual. In “The Upside of Stress,” Kelly McGonigal defines stress as a physiological response to a perceived threat or challenge (4). It’s a natural reaction designed to help us cope with demands and uncertainties- so it’s not an inherently bad feeling, but rather a tool that can be used to enhance our lives when managed effectively.
McGonigal differentiates between two types of stress responses:
Threat Response
This occurs when we perceive a situation as dangerous and our bodies react in a fight-or-flight mode. When this response is triggered, we see an increase in cortisol levels which is linked to slower wound and tissue healing (3) and various other health conditions.
Challenge Response
This happens when we view a situation as an opportunity for growth and our bodies respond with increased focus and energy. DHEA, a neurosteroid, is elevated when stress is perceived positively. This can accelerate wound healing, enhance immune function, and decrease the risk of various stress-related health problems, including anxiety, depression, heart disease, and neurodegeneration.
For the majority of the population, sustaining an injury will trigger our threat stress response, which is completely understandable. What many studies and Dr. McGonigal have found though, is we promote healing and overall improved well-being if we can shift these experiences to a challenge stress response.
Here are recommendations on how you can do that:
- Mindfulness and Meditation: These practices can help you become more aware of your thoughts and feelings, reducing the impact of negative stress responses.
- Cultivate a Growth Mindset: By viewing challenges as opportunities for growth, you can shift your perspective and reduce the stress associated with threats. Most of the time, injuries allow us to rebuild a stronger foundation of movement- so you can view the rehabilitation process as an opportunity to become stronger and more resilient! (5)
- Social Connection: Strong social bonds can provide support and resilience in stressful situations.
- Physical Activity: Exercise has been shown to reduce stress and improve overall well-being. Incorporating breath work into this also helps calm the nervous system and reduce pain perception. This is where your physical therapist thrives- we help determine which exercise or activity is best suited for your current physical and mental state.
- Healthy Lifestyle: Prioritizing sleep, nutrition, and relaxation can help manage stress. Balance is hard in our busy lives and juggling all these factors can be daunting- if you can be 80% performant on these variables though, you’re living the dream!
- Challenge Yourself Gradually: Start with small, manageable challenges to build resilience and confidence. In physical therapy, we establish personal short and long term goals with continual measuring of progress along your healing journey.
- Reframe Stressful Thoughts: Instead of focusing on negative aspects of a situation, try to find positive perspectives or opportunities for growth.
Understanding the distinction between pain and discomfort is vital for athletes navigating the complexities of injury and recovery. By effectively managing both sensations through strategies like RPE and stress management techniques, athletes can optimize their performance, minimize the risk of burnout, and ultimately enhance their overall well-being.
Remember, the journey to recovery is not just about physical healing but also about cultivating a resilient mindset and fostering a positive relationship with stress.
References
- Morishita S, Tsubaki A, Takabayashi T, Fu JB. Relationship between the rating of perceived exertion scale and the load intensity of resistance training. Strength Cond J. 2018 Apr;40(2):94-109. doi: 10.1519/SSC.0000000000000373. PMID: 29674945; PMCID: PMC5901652.
- van Winden D, van Rijn RM, Savelsbergh GJP, Oudejans RRD, Stubbe JH. The Association Between Stress and Injury: A Prospective Cohort Study Among 186 First-Year Contemporary Dance Students. Front Psychol. 2021 Nov 5;12:770494. doi: 10.3389/fpsyg.2021.770494. PMID: 34803856; PMCID: PMC8602075.
- Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011 Feb;31(1):81-93. doi: 10.1016/j.iac.2010.09.010. PMID: 21094925; PMCID: PMC3052954.
- McGonigal K. The Upside of Stress : Why Stress Is Good for You, and How to Get Good at It. Avery, a member of Penguin Random House; 2015.
- Neumann RJ, Ahrens KF, Kollmann B, Goldbach N, Chmitorz A, Weichert D, Fiebach CJ, Wessa M, Kalisch R, Lieb K, Tüscher O, Plichta MM, Reif A, Matura S. The impact of physical fitness on resilience to modern life stress and the mediating role of general self-efficacy. Eur Arch Psychiatry Clin Neurosci. 2022 Jun;272(4):679-692. doi: 10.1007/s00406-021-01338-9. Epub 2021 Oct 7. PMID: 34622343; PMCID: PMC9095527.







