I recently received a before-and-after picture from one of my patients. It was a picture of her foot before starting physical therapy, next to a picture of her foot a few months into physical therapy.
This patient had been seeing me for a myriad of issues. After her assessment, I found that many of the pain issues she was experiencing stemmed from a lack of mobility in her toes, foot, and ankle. Sure enough, one of the issues that had been bothering her was the painful bunion on her foot. She told me that her symptoms were occasional but worsened with activity, and she was concerned about her bunion progressing.
“My grandma had severe bunions, and I am afraid I inherited her feet!” she told me.
After 4 sessions, her bunion visibly improved, and her pain disappeared. Why? Because she acted early, focused on prevention, and committed to a simple, tailored exercise and treatment program.

The before and after picture of one of my patient’s feet. The picture on the Left was taken prior to them starting physical therapy. The picture on the Right was after 4 sessions of physical therapy.
Bunions don’t have to mean surgery. This blog post outlines what you need to know about what bunions really are, the myths surrounding them, and how a physical therapist can help you keep moving with less pain.
What Exactly Is a Bunion?
Hallux valgus, or bunion, is a common progressive foot deformity resulting in abnormal angulation of the big toe and its joint, causing a bony prominence. Bunions can begin as a bump on the inner foot and, untreated, progress to painful disability and difficulty walking.
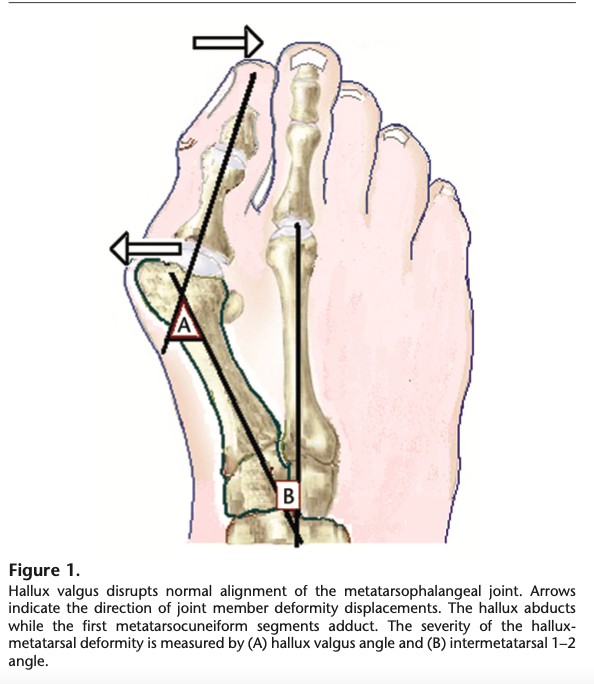
From Glasoe WM, Nuckley DJ, Ludewig PM. Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Phys Ther. 2010;90:110-120.
Bunions are most prevalent in women, affecting 35% of those over 65 years of age. They become more common as we get older. Athletes also face a higher risk. For example, 36-55% of dancers are affected by the condition.
While we don’t really know why people get bunions, there are several risk factors that contribute to the development of the deformity, including:
- Genetics
- Ill-fitting footwear
- Other foot deformities, such as flat feet
- Trauma
- Arthritis
- Muscle imbalances
- Poor biomechanics
- Joint laxity
It is believed that bunions are caused by imbalances within the muscles of the foot and ankle, which alter the biomechanics of the foot. This alteration leads to increased tissue stress in the base of the great toe, stimulating bone growth and forming a bunion. The swollen area can become painful, further aggravating the condition and leading to further disruptions in walking mechanics.
Symptoms of hallux valgus include:
- Pain or swelling at the bunion
- Stiffness or reduced mobility of the big toe
- Difficulty finding shoes that fit comfortably
If left untreated, bunions can cause pain that affects walking, standing, and even your hips, knees, and back. The longer they progress, the more they alter your body’s mechanics, making treatment harder later.

Can You Actually Prevent Bunions
You can’t always prevent bunions, but you can often slow their progression.
Targeting certain muscles of the foot and ankle can slow the progression of the deformity and optimize the biomechanics of the foot. Therefore, the goal is to prevent the progression of bunions, so the deformity does not become so severe that surgery is required.
There are two groups of muscles in the foot:
- Intrinsic foot muscles (muscles that do not cross the ankle joint) are responsible for maintaining arch support and assist in holding the toes on the ground.
- Extrinsic foot muscles (muscles that cross the ankle joint) power walking.
Together, these muscle groups distribute weight across the ball of the foot and propel us as we stand, walk, or run.
Bunions alter how these groups of muscles work together, shifting most of the work to the extrinsic foot muscles. This added workload increases biomechanical stress on the big toe and contributes to a flatfoot posture. As biomechanical stress increases, the deformity worsens, and the intrinsic foot muscles become weak. These changes in pressure across the foot contribute to other lower limb pain issues, including tibial tendonitis, patellofemoral pain, and hip pain.
That’s why strengthening the right muscles, improving mobility, and correcting biomechanics are so important.
Surgery is sometimes needed, but it isn’t a guaranteed fix. In fact, studies show bunions return in up to 40% of cases after surgery.
Common Treatments for Bunions
Conservative interventions are always recommended first when treating hallux valgus. Common treatments include:
- NSAIDs
- Physical therapy
- Corrective orthotics
- Wide box or protective shoe wear
- Splinting
- Taping
- Injections
Most of these interventions address the biomechanical causes of the deformity and are effective at reducing pain and improving mobility.
Surgery is recommended only if conservative therapy fails, pain or dysfunction persist and affect activity, shoes no longer fit, there are cosmetic concerns, or in late-stage deformity. Over 100 surgeries exist, varying by surgeon. Recovery takes eight weeks or more, and postoperative physical therapy is crucial to restore motion. Delaying surgery for conservative treatment does not worsen outcomes.

Bunion Myths That Need Busting
Myth 1: Surgery is the only effective treatment
Truth: Conservative treatments, such as physical therapy, foot orthotics, night splints, dynamic splints/toe separators, and Botox injections, have all been shown to improve bunion-associated pain and enhance function.
Non-surgical treatments should be trialed before surgery, especially in the early stages of hallux valgus, to maintain muscle strength, improve biomechanics, and reduce foot pain.
Myth 2: Bunions only happen because of bad shoes
Truth: Bunions are caused by altered biomechanical forces in the foot. If these forces are not corrected, the deformity will progress. While shoe choice can contribute to the formation of a bunion, other factors also contribute to its development, including genetics, existing foot deformities such as flat feet, trauma, arthritis, muscle imbalances, poor biomechanics, and joint laxity.
Myth 3: Once you fix it surgically, it never comes back
Truth: While surgery is the only way to cosmetically fix a late-stage bunion, recurrence rates of bunions after surgery are high, anywhere from 15-40% depending on the study. Physical therapy is often recommended following surgery to restore range of motion, joint mobility, and foot strength.
Myth 4: PT can’t help (it’s a bone issue)
Truth: Physical therapist interventions, including exercise and manual therapy, are very effective in treating hallux valgus. While the bone is what forms a bunion, it becomes more prominent due to imbalances in the various muscles of the foot and ankle. The increased pull of extrinsic muscles on the joint, coupled with less tension from the intrinsic muscles of the foot, leads to the base of the big toe shifting outward.
This biomechanical change is then exacerbated during walking, resulting in additional biomechanical stresses on the big toe. Physical therapists offer treatments to restore muscle balance in the foot and ankle, enhance mobility during gait, and reduce biomechanical stressors that exacerbate the deformity. The earlier the problem is addressed, the better the outcomes.
How Physical Therapy Fixes The Root Cause
Biomechanical assessment like gait, alignment, mobility, and strength.
Strengthening exercises target the intrinsic muscles of the foot including:
- Abductor hallucis (this is the only muscle that prevents the great toe from shifting to form the deformity of hallux valgus)
- Adductor hallucis (this muscle provides counterbalance to the abductor hallucis and promotes proper alignment of the big toe)
- Flexor hallucis brevis (this muscle moves the big toe downward and supports the foot’s arch).
Strengthening tibialis posterior and fibularis longus (extrinsic muscles) supports the midfoot, arch, and limits pronation.
Manual therapy like joint mobilizations and soft tissue work improve mobility of the big toe, ankle, knee, and hip.
As a bunion progresses, joint mobility and range of motion worsen. Joint mobilizations combined with stretching can help improve the mobility and flexibility of joints and muscles that may be contributing to poor biomechanics.
Footwear and activity advice on how to load without aggravating symptoms.
Physical therapists provide individualized recommendations for footwear, taping techniques, bracing, and activity modifications to reduce biomechanical stressors on the foot.
Neuromuscular re-education on retraining walking mechanics.
Physical therapists are trained to determine how other joints and muscles contribute to the primary pain or biomechanical problem, so these factors will be considered during the assessment and treatment plan.
PTs can provide guidance on modification of gait mechanics to prevent progression of the deformity with ambulation, standing, or running activities.
Prehab & Post-op rehab to prepare for and recover from surgery.
If surgery is required, physical therapists can prepare a person’s body for surgery, enabling them to enter the operating room with improved mobility and strength, which in turn leads to better outcomes.
Post-operative rehab is recommended following surgery to restore range of motion, mobility, and strength for optimal recovery.

Exercises to Help Your Bunions Right Now
These are the exercises I most frequently recommend to patients with bunions. I always suggest starting the exercises in a sitting position to learn proper movement, and then progress to standing on both feet, and finally, one foot if it is safe to do so.
Exercises should go to fatigue. All exercises are held with maximum effort for 5 seconds. Eventually, you will want to apply these to your daily life.
- Towel Scrunches
- Toe Yoga
- Toe Spreading
- Arch Lifting
- Gastroc Stretch on Wall
- Soleus Stretch on Wall
- Standing Heel Raises
Here are descriptions for how to perform each exercise above.
1 – Towel Scrunches
- Reps: 30
- Sets: 1
- Daily: 1
- Weekly: 7
Setup
Begin in a staggered standing position with your forward foot resting on a flat towel, and the knee slightly bent.
Movement
Keep your back knee straight. Moving at the ball of your foot, use your toes to scrunch up the towel.
Tip
Make sure to keep the rest of your foot in contact with the ground.
2 – Toe Yoga
Alternating great toe and lesser toe extension.
- Reps: 30
- Sets: 1
- Daily: 1
- Weekly: 7
Setup
Begin sitting upright in a chair with your feet resting flat on the floor. Remove the shoe on your affected foot.
Movement
Lift your big toe straight up, keeping your other toes flat on the ground. Then, keeping your big toe on the ground, lift your four smaller toes up into the air. Pause, then return to the starting position. Repeat.
Tip
Make sure to keep the muscles in the arch of your foot active during the exercise. Make sure not to dig your toes into the ground to complete the motion.
3 – Toe Spreading
- Reps: 30
- Sets: 1
- Daily: 1
- Weekly: 7
Setup
Begin in a standing upright position with your feet shoulder width apart, looking down at your feet.
Movement
Gently spread your toes apart to cause the arch of your foot to rise away from the ground.
Tip
Make sure to keep your foot in contact with the ground.
4 – Arch Lifting
- Reps: 30
- Sets: 1
- Daily: 1
- Weekly: 7
Setup
Begin in a staggered standing position with your front knee slightly bent and your back knee straight.
Movement
Try to lift up the arch of your foot while keeping your toes and heel in contact with the ground.
Tip
Make sure to avoid gripping with your toes. A slight weight shift to the outside of your foot is normal.
5 – Gastroc Stretch on Wall
- Reps: 20
- Sets: 1
- Hold: 5 seconds
- Daily: 1
- Weekly: 7
Setup
Begin in a standing upright position in front of a wall.
Movement
Place your hands on the wall and extend one leg straight backward, bending your front leg, until you feel a stretch in the calf of your back leg and hold.
Tip
Make sure to keep your heels on the ground and back knee straight during the stretch.
6 – Soleus Stretch on Wall
- Reps: 20
- Sets: 1
- Hold: 5 seconds
- Daily: 1
- Weekly: 7
Setup
Begin in a standing upright position in front of a wall.
Movement
Place your hands on the wall and extend one leg backward with your knee bent. Lean forward into the wall, until you feel a stretch in your lower calf and hold.
Tip
Make sure to keep your heels on the ground and back knee bent during the stretch.
7 – Heel Raises
- Reps: 10
- Sets: 2
- Daily: 1
- Weekly: 7
Setup
Begin in a standing upright position in front of a counter or stable surface for support.
Movement
Slowly raise both heels off the ground as you increase the weight into your big toes, then lower your heels down to the floor and repeat.
Tip
Make sure to maintain an upright posture and keep your weight on the balls of your feet when you lift your heel
If these feel painful or you’re unsure, a PT can customize the plan for your foot.
Final Thoughts
Like my patient who saw her bunion pain disappear in just four sessions, you don’t have to wait until surgery feels like your only option.
Bunions are common, but early physical therapy often reduces pain, improves function, and helps you avoid surgery.
At MovementX, we provide personalized, convenient, and expert care that assesses your biomechanics from head to toe, allowing us to prevent the progression of musculoskeletal problems like bunions, so you can move better and live pain-free.
If you have a bunion that is painful or limiting your activity level, set up an appointment today!
References
- DeCaro LJ, Nole R, Coletta J, Bowie D, Filipiak D. A multidisciplinary approach to managing bunion deformity in the overly pronated foot. Podiatry Management. 2009. 147-151.
- Glasoe WM, Nuckley DJ, Ludewig PM. Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Phys Ther. 2010;90:110-120.
- Glasoe WM. Treatment of Progressive First Metatarsal Hallux Valgus Deformity: A Biomechanically Based Muscle Strengthening Approach. J Ortho Sports Phys Ther. 2016: 46;7. 596-605.
- Hernandez-Castillejo LE, Martinez Vzcaino V, Garrido-Miguel M et al. Effectiveness of hallix valgus surgery on patient quality of life: a systematic review and meta-analysis. Acta Orthopaedica. 2020; 91 (4): 450-456.
- Hurn SE, Matthews BG, Munteanu SE, Menz HB. Effectiveness of Nonsurgical Interventions for Hallux Valgus: A Systematic Review and Meta-Analysis. Arthritis Care Res (Hoboken). 2022 Oct;74(10):1676-1688. doi: 10.1002/acr.24603. Epub 2022 Jun 17. PMID: 33768721.
- Hwang BH & Jeon IC. Comparison of abductor hallucis muscle activity in subjects with mild hallux valgus during three different foot exercises. J Back Musculoskel Rehabil. 2024; 37: 47-54. DOI 10.3233/BMR-220252.
- Liu Z, Zhong Y, Chen S, Tanaka H et al. Effects of 4 weeks of foot exercise on subjective outcome and foot plantar pressure in elite adolescent dancers with hallux valgus: a pilot study. BMC Sports Sci Med and Rehab. 2024; 16:217-230.
- Tedeschi R. Exploring the Efficacy of Physiotherapy in Conservative Management of Hallux Valgus: A Scoping Review of Randomized Clinical Trials. Reabilitacijos Mokslai: slauga, kineziterapija, ergoterapija, 2 (31) 2024, 24–32, eISSN 2538-8673; DOI: https://doi.org/10.33607/rmske.v2i31.1532.
- Tokki M, Malmivaara A, Seitsalo S et al. Hallux valgus: immediate operation versus 1 year of waiting with or without orthoses. Acta Orthop Scand. 2003; 74(2): 209-215.








