In today’s healthcare system, patients are increasingly frustrated by long wait times, rising costs, and fragmented care. The average wait to see a new physician in the U.S. is 26 days—and for specialists like orthopedists, that number climbs even higher. Out-of-pocket expenses continue to rise, especially with high-deductible plans, causing many people to delay treatment until problems worsen.
Musculoskeletal conditions like back pain, joint dysfunction, and sports injuries are among the most common—and costly—reasons people seek care, accounting for over $380 billion annually in U.S. healthcare spending. Yet despite strong evidence for conservative care, most patients are still funneled through urgent care, imaging, or specialty referrals before anyone addresses the root of the problem—how they move.
For musculoskeletal pain, starting with a physical therapist often leads to faster relief, fewer procedures, and better long-term outcomes—while keeping your primary care provider as an essential partner in your care.
The Case for Physical Therapy as First-Line Care
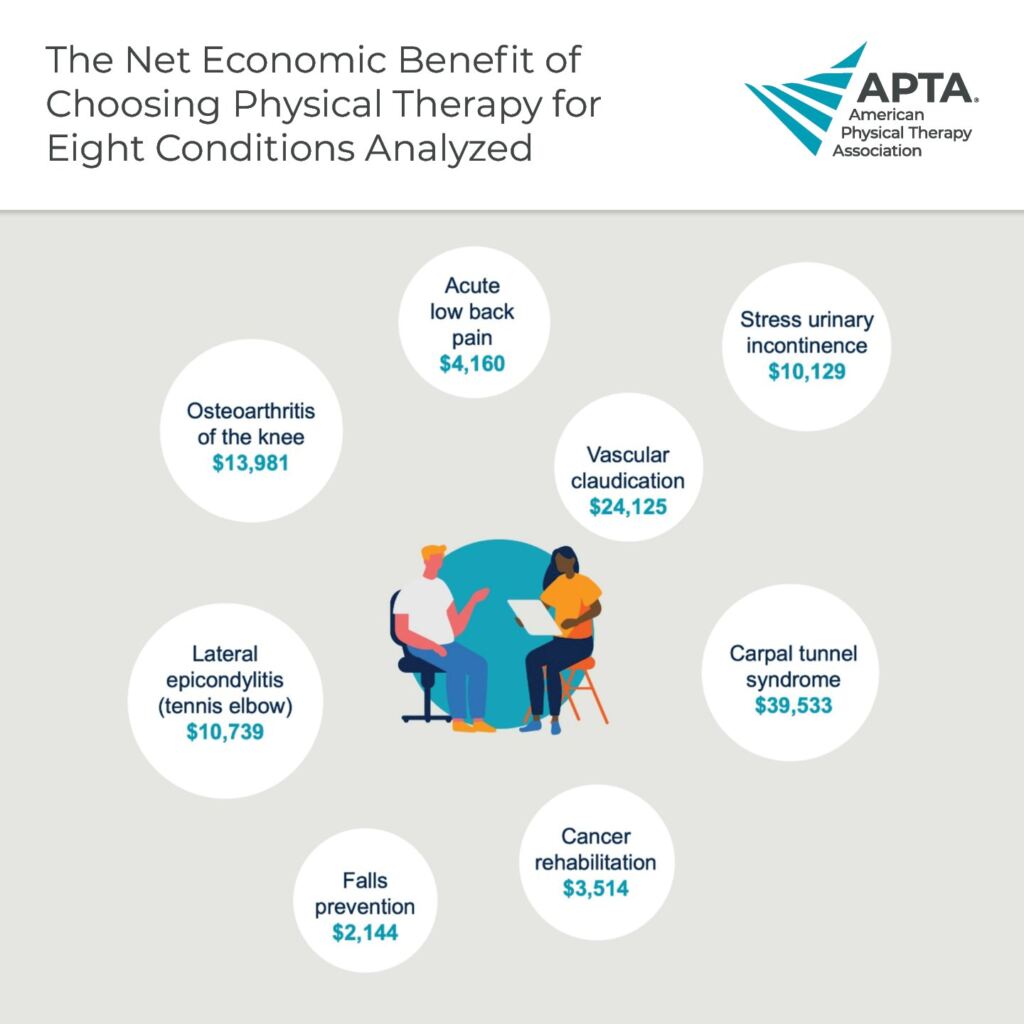
Research shows that early access to physical therapy leads to better outcomes, faster recovery, and substantial cost savings:
- Patients with low back pain who saw a physical therapist first saved an average of $1,500 to $2,700 per episode of care.
- Early PT is associated with:
- 28% fewer imaging studies
- 33% fewer spinal injections
- 32% lower surgery rates
- 89% lower odds of opioid use
Physical therapists are movement experts trained to evaluate, diagnose, and treat musculoskeletal conditions—often without the need for a referral. By offering evidence-based care at the point of pain, they help patients avoid unnecessary imaging, medications, or surgeries that delay progress and drive up costs.
Still, most people first visit a PCP, urgent care, or walk-in orthopedic clinic—settings where PT is too often an afterthought, not the starting point.
Direct Access Physical Therapy in DPC: Faster, Smarter Care for Pain and Injury
Direct Primary Care (DPC) is built on accessibility, affordability, and proactive treatment—making it an ideal setting for early physical therapy intervention.
Patients benefit from more time with their providers, same-day access, and fewer barriers to care.
Within this model, physical therapy isn’t just a support service—it’s a strategic first-line solution for musculoskeletal health. By partnering with physical therapists, DPC practices create a collaborative, whole-person care experience that delivers faster recovery, fewer interventions, and long-term value for patients.
5 Ways Physical Therapists Improve Primary Care Outcomes
- Prevent Escalation with Early, Direct Access Treatment
Musculoskeletal issues often worsen with time and inactivity. Physical therapy provides immediate evaluation and treatment, helping patients avoid unnecessary imaging, medications, or surgery—without the need for referral. - Manage Pain Without Medication or Side Effects
PTs use exercise, manual therapy, and movement retraining to manage pain without the use of opioids or other pharmaceuticals—critical in today’s effort to reduce medication reliance. - Address the Root Cause with Whole-Person Assessment
Physical therapists assess posture, biomechanics, lifestyle, and activity patterns to treat root causes—not just symptoms. This holistic approach aligns seamlessly with DPC’s patient-centered model. - Cut Healthcare Costs with Conservative, Proactive Care
With no need for referrals, approvals, or complex billing systems, PT care can be initiated quickly and affordably—often resulting in faster resolutions and lower total healthcare spending. - Collaborate Seamlessly with Primary Care Providers
PTs work closely with primary care physicians to co-manage patient needs, monitor outcomes, and ensure continuity of care without duplication or delay.

Physical Therapists vs. Primary Care, Chiropractors, and Surgeons: Who Should You See First for Pain?
Education and Expertise
To practice, physical therapists must earn a Doctor of Physical Therapy (DPT) degree—a rigorous, three-year program beyond a bachelor’s degree. Their training includes:
- Musculoskeletal anatomy and biomechanics
- Pain science and neuroscience
- Manual therapy and therapeutic exercise prescription
- Clinical reasoning and differential diagnosis
This gives PTs a deep understanding of movement systems and functional recovery—skills not often emphasized in other healthcare professions.
How PT Training Compares
| Provider | Musculoskeletal Focus | Strengths | Limitations |
| Physical Therapist (DPT) | Highly specialized | Non-surgical rehab, movement assessment, exercise prescription | Cannot prescribe medication (or imaging in most states) |
| Primary Care Physician | General knowledge | Whole-body health, referrals | Limited hands-on or movement-based training |
| Orthopedic Surgeon | Surgical expertise | Complex diagnosis, surgical intervention | Enters care later; limited conservative treatment |
| Chiropractor | Spinal and manual care | Adjustments, pain management | Narrower scope; less emphasis on active rehabilitation |
Common Conditions Physical Therapy Can Help—Without Surgery or Medication
Physical therapists treat a wide range of musculoskeletal issues, including:
- Low Back and Neck Pain: From acute strain to chronic disc and nerve issues
- Joint Pain and Arthritis: Knee, hip, shoulder, and spine
- Sports Injuries: Sprains, tendinopathies, overuse injuries
- Post-Surgical Rehabilitation: Joint replacements, ACL repairs, spinal surgeries
- Chronic Pain Conditions: Fibromyalgia, CRPS, and other complex cases
Case Study Example: Youth Athlete
A 10-year-old baseball player reported knee pain after performing repeated squats in a speed and agility class. Despite still being able to bear weight through his leg, his parents were concerned and took him to a local medicine walk-in clinic for evaluation. After negative x-ray findings and a brief physical examination, the patient was placed on crutches and told he would eventually need an MRI. No therapy plan was given.
After three weeks of being on crutches, the patient’s pain had not improved. Frustrated by the lack of progress and baseball season quickly approaching, his parents called a physical therapist who was able to see him on the same day. After the evaluation, the physical therapist determined that the boy would benefit from immediate conservative treatment and recommended that the parents hold off on the MRI as any potential for surgery was not warranted at the time, and any findings were unlikely to change the current plan of care.
In less than two weeks of initiating physical therapy, the patient was back to running and batting, pain-free. His parents cancelled the MRI altogether, saving them more than $400, and he participated in his first game of the season just eight weeks after the injury. Had physical therapy been prescribed earlier, the patient would have return to activity much sooner and may have resulted in even fewer healthcare costs.

Takeaway: Movement Is Medicine—Start with Physical Therapy First
Direct access to physical therapy offers a smarter, more cost-effective path to musculoskeletal health. PTs provide timely, evidence-based, and personalized care that prevents escalation, reduces costs, and helps patients return to the activities they love—faster and safer.
If you’re dealing with pain, discomfort, or movement limitations, your first step shouldn’t be imaging, injections, or waiting weeks for a specialist.
Your first step toward lasting relief likely isn’t surgery or scans—it might just be smarter movement.
References
- American Physical Therapy Association. (n.d.). The value of physical therapy: Facts & figures. Retrieved from https://www.apta.org
- Fritz, J. M., Childs, J. D., Wainner, R. S., & Flynn, T. W. (2012). Primary care referral of patients with low back pain to physical therapy: Impact on future health care utilization and costs. Health Services Research, 47(2), 819–839. https://doi.org/10.1111/j.1475-6773.2011.01324.x
- Kazis, L. E., Ameli, O., Rothendler, J., Garrity, B. H., Murtaugh, C. M., Zafar, S. Y., & Cabral, H. J. (2019). Observational retrospective study of the association of initial healthcare provider for new-onset low back pain with early and long-term opioid use. BMJ Open, 9(6), e028633. https://doi.org/10.1136/bmjopen-2018-028633
- Mafi, J. N., McCarthy, E. P., Davis, R. B., & Landon, B. E. (2013). Worsening trends in the management and treatment of back pain. JAMA Internal Medicine, 173(17), 1573–1581. https://doi.org/10.1001/jamainternmed.2013.8992
- Martin, B. I., Deyo, R. A., Mirza, S. K., Turner, J. A., Comstock, B. A., Hollingworth, W., & Sullivan, S. D. (2008). Expenditures and health status among adults with back and neck problems. JAMA, 299(6), 656–664. https://doi.org/10.1001/jama.299.6.656
- Peterson, C., Grosse, S. D., & Dunn, A. (2021). Economic burden of musculoskeletal disorders in the United States: Estimates from the MEPS. Medical Care, 59(11), 965–972. https://doi.org/10.1097/MLR.0000000000001620
- Zhu, J. M., et al. (2021). Trends in primary care visit use and content, 2002–2015. JAMA Internal Medicine, 181(1), 108–110. https://doi.org/10.1001/jamainternmed.2020.3987
About the Author
Dr. Adam Kays is a physical therapist and Board-Certified Orthopedic Clinical Specialist in Central Indiana. Among Adam’s treatment specialities are spine disorders, headaches, trigeminal neuralgia, and dry needling. Dr. Adam believes in empowering his patients through education and exercise self-efficacy to help you return to your favorite fitness activities better than before.








