Sleep Well, Move Well, Live Well: The Role of Physical Therapy in Sleep Apnea Management
Not only are we as Americans collectively sleep deprived (over one third of adults don’t get the recommended 7-9 hours of sleep per night) but 50-70 million US adults also suffer from chronic sleep disorders which negatively impact the quality of their sleep [5]. One of the most prevalent and dangerous of these sleep disorders is obstructive sleep apnea (OSA) which is estimated to affect over 20% of American adults, the majority of whom are undiagnosed [16]. Many of us feel like we are doing all of the right things but still wake in the morning feeling tired and unrested which can really get in the way of living our best life.
Great sleep is important for many aspects of our health including healing, pain modulation, cognitive function, metabolic function, cardiovascular health, and modulating anxiety and depression. If something regularly disrupts the quality of our sleep it can set off a whole cascade of negative health issues. This article will explore sleep apnea and its effect on a person’s health along with the role of physical therapy in the management of obstructive sleep apnea.

Obstructive Sleep Apnea
Obstructive sleep apnea is characterized by a partial or complete collapse of the upper airway resulting in decreased oxygen saturation due to temporary reduction in breathing (hypopnea) or cessation of breathing (apnea). The diagnostic measure for sleep apnea is the apnea-hypopnea index (AHI) which measures the number of instances of apnea or hypopnea per hour of sleep and is measured by a sleep study at a facility or at-home sleep testing.
Apnea-Hypopnea Index (AHI) Criteria
Normal: <5 events/hour
Mild OSA: 5-15 events/hour
Moderate OSA: 15-30 events/hour
Severe OSA: >30 events/hour
Thankfully when apnea or hypopnea occurs, our brain senses the decrease in oxygen level and triggers a failsafe reflex to arouse a person from sleep so that they resume breathing. However, these frequent arousals result in significantly diminished quality of restorative sleep. Common symptoms of obstructive sleep apnea include:
- Fatigue even after a full night sleep
- Daytime sleepiness
- Snoring
- Impaired memory and concentration
- Mood changes
- Insomnia
- Night sweats
- Frequent urination during the night
- Morning headache
- Sexual dysfunction
As you might expect, there are also numerous factors that can contribute to increased risk of obstructive sleep apnea such as family history, increased neck size, increased age and postmenopause, sex (men are at a greater risk than women), being overweight or obese, chronic nasal congestion, smoking and alcohol consumption, and other concurrent conditions such as thyroid problems and Down Syndrome.
Remember, the vast majority of sleep apnea cases are undiagnosed (up to 80% of people with OSA are undiagnosed [1]) and develop over time. It is important for anyone exhibiting the symptoms and risk factors associated with sleep apnea to discuss them with an appropriate healthcare provider. If left untreated, sleep apnea can lead to other health problems such as continued change in mental function, increased blood pressure, impaired metabolic function, and increased risk for heart arrhythmias, heart failure, and stroke.
Conventional Treatment
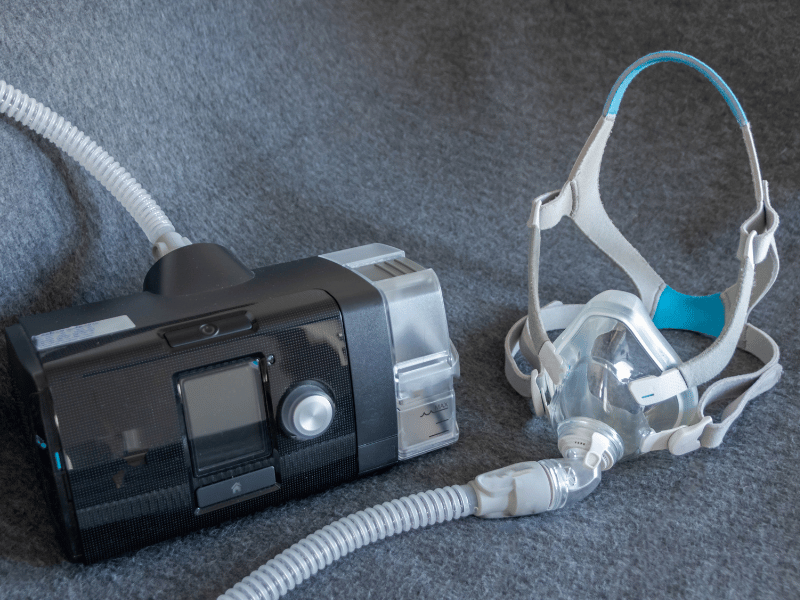
A gold standard treatment for obstructive sleep apnea has been and remains use of a continuous positive airway pressure or CPAP machine which uses air pressure to prevent your airway from collapsing while sleeping. The field of dental sleep medicine has also grown significantly with dentists providing home sleep testing and using devices to keep the airway open by advancing the mandible or stabilizing the tongue. In severe cases or when indicated patients may undergo a number of different surgical procedures to address the airway problems contributing to their sleep apnea. It is also very common for multiple different providers to aid in many other aspects of treatment. Providers involved in the management of sleep apnea can include medical specialists (primary care, sleep, otolaryngology, pulmonology, cardiology, neurology, psychology/psychiatry, dental specialists (general dentistry, orthodontics, and oral surgery), dieticians, respiratory therapists, and physical therapists.
The Role of PT in Sleep Apnea Treatment
According to current practice standards, sleep health falls within the scope of practice for physical therapists who can assess sleep quality and screen for dysfunction, identify impairments related to sleep dysfunction, implement therapeutic interventions to address impairments that interfere with sleep, educate patients on sleep hygiene, incorporate sleep-promoting strategies into treatment plans, and refer patients to other specialists as appropriate.
Physical therapy is not intended to replace traditional sleep apnea treatments but function as an excellent complementary or adjunctive treatment that can help OSA patients achieve enhanced treatment success and better health outcomes. Below are ways in which a physical therapist can be an integral player in the management of obstructive sleep apnea.
Physical Activity and Weight Loss
Physical therapists are movement experts and are well equipped to safely guide OSA patients through a customized physical exercise program. Numerous forms of physical activity have been found to improve a person’s apnea-hypopnea index. As expected aerobic exercise is very beneficial for OSA patients and has been found to reduce AHI by up to 32% [10]. However, research has also found reductions in AHI with other forms of exercise as well including strength training in older adults and high intensity interval training in obese children.
Additional studies show that combinations of exercise types such as resistance training in addition to aerobic exercise are more effective than just one form of exercise [13]. Physical activity is also beneficial for weight loss. Body weight has been found to correlate with sleep apnea incidence and a 5-10% weight loss can result in a decrease in AHI of up to 26% [18].
Respiratory Muscle Training
Another treatment that has been found to improve obstructive sleep apnea is breathing retraining exercises or respiratory muscle training. Within this form of treatment there are multiple approaches including diaphragmatic breathing, Buteyko breathing, inspiratory resistance training and even consistent completion of intensive, repetitive activities such as singing or playing a wind instrument.
Respiratory muscle therapy has been found to improve AHI by up to 39.5% [9]. Respiratory training contributes to improvements in muscle tone of the upper airway, respiratory muscle strength, neuroplasticity of breathing control, oxygen levels, hyperventilation/breathing dysfunction, and autonomic nervous system, metabolic, and inflammatory status.
Postural Therapy
In addition to plenty of information on sleep hygiene, physical therapists can provide postural education and strategies to optimize breathing while sleeping. Sleeping on one’s back can lead to increased likelihood of airway collapse or the tongue falling back and obstructing the airway. It’s estimated that 60% of people with OSA have positional OSA. A simple change to sidesleeping can reduce AHI by up to 40-50% [11]. Physical therapists can provide education and treatment to improve daytime posture, rib cage expansion, and postural strength to optimize breathing during the day and at night.
Orofacial Exercises/Myofunctional Therapy
Myofunctional therapy is a specialized treatment approach involving a series of exercises aimed at improving muscle coordination, improving breathing patterns, and correcting tongue posture to achieve proper function of the oral and facial muscles as well as alignment of the jaw and facial structure. Research has found that myofunctional therapy improved oxygen saturation level, snoring, sleep outcomes, and improved AHI by up to 50% in adults and 62% in kids [4]. Additionally, it was found that patients completing myofunctional therapy are more likely to be compliant with CPAP conventional treatment [8].
If seeking myofunctional therapy it is important to find a therapist who has completed adequate training.

Conclusion
Living well can be a challenge. We all have busy schedules that are quickly filled with work, family, and the rest of life’s demands. So why not make the most out of the one thing that we all do every day. Break free from the epidemic of poor sleep that plagues so many of us and get the care that you need to get the most out of your sleep each night. If you want to live well you have to sleep well.
MovementX has physical therapists with a wide range of specialties across the United States. Click here to find a PT who can help you get better sleep today.
References
- American Academy of Sleep Medicine. Sleep Apnea. American Academy of Sleep Medicine; 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf. Accessed November 13, 2024.
- American Physical Therapy Association. From PTJ: PTs should wake up to their role in promoting sleep health. American Physical Therapy Association. Published August 8, 2017. Accessed November 13, 2024. https://www.apta.org/news/2017/08/08/from-ptj-pts-should-wake-up-to-their-role-in-promoting-sleep-health
- Andrade FM, Pedrosa RP. The role of physical exercise in obstructive sleep apnea. J Bras Pneumol. 2016;42(6):457-464. doi:10.1590/S1806-37562016000000156
- Camacho M, Certal V, Abdullatif J, et al. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. Sleep. 2015;38(5):669-675. Published 2015 May 1. doi:10.5665/sleep.4652
- Centers for Disease Control and Prevention. Prevalence of Chronic Obstructive Pulmonary Disease Among Adults — United States, 2019–2020. Prev Chronic Dis. 2023;20:220400. Published August 3, 2023. Accessed November 7, 2024. https://www.cdc.gov/pcd/issues/2023/22_0400.htm.
- Cleveland Clinic. Sleep Apnea. Cleveland Clinic. Updated July 12, 2023. Accessed November 13, 2024. https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
- Courtney R. Breathing retraining in sleep apnoea: a review of approaches and potential mechanisms. Sleep Breath. 2020;24(4):1315-1325. doi:10.1007/s11325-020-02013-4
- de Felício CM, da Silva Dias FV, Trawitzki LVV. Obstructive sleep apnea: focus on myofunctional therapy. Nat Sci Sleep. 2018;10:271-286.
- Hsu B, Emperumal CP, et al. Effects of respiratory muscle therapy on obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2020;16(5):785-801. doi:10.5664/jcsm.8318
- Iftikhar IH, Kline CE, Youngstedt SD. Effects of exercise training on sleep apnea: a meta-analysis. Lung. 2014;192(1):175-184. doi:10.1007/s00408-013-9511-3
- Lee JI, Choi KH. Positional Therapy for Obstructive Sleep Apnea: Therapeutic Modalities and Clinical Effects. Sleep Med Res. 2023;14(3):129-134.
- National Heart, Lung, and Blood Institute. Sleep Deprivation and Deficiency. National Institutes of Health. Updated August 30, 2023. Accessed November 7, 2024. https://www.nhlbi.nih.gov/health/sleep-deprivation.
- Peng J, Yuan Y, Zhao Y, Ren H. Effects of Exercise on Patients with Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19(17):10845. Published 2022 Aug 31. doi:10.3390/ijerph191710845
- Siengsukon CF, Al-Dughmi M, Sharma NK. A survey of physical therapists’ perception and attitude about sleep. J Allied Health. 2015;44(1):41-50.
- Siengsukon CF, Al-Dughmi M, Stevens S. Sleep Health Promotion: Practical Information for Physical Therapists. Phys Ther. 2017;97(8):826-836. doi:10.1093/ptj/pzx057
- Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. [Updated 2024 Mar 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459252/
- Strohm M, Daboul A, Obst A, Weihs A, Busch C-J, Bremert T, Fanghänel J, Ivanovska T, Fietze I, Penzel T, et al. Association Between Sleep Position, Obesity, and Obstructive Sleep Apnea Severity. Journal of Personalized Medicine. 2024; 14(11):1087. https://doi.org/10.3390/jpm14111087
- Wolk R, Shamsuzzaman AS, Somers VK. Obesity, sleep apnea, and hypertension. Hypertension. 2003;42(6):1067-1074. doi:10.1161/01.HYP.0000101686.98973.A3








