Newly Diagnosed with Parkinson’s Disease? 3 Essential Next Steps
Receiving a diagnosis of Parkinson’s Disease can evoke a whirlwind of emotions. You might feel shock, uncertainty about your future, or even relief at finally having answers for symptoms that have puzzled you for years. Whatever you’re feeling, know that these emotions are valid and they won’t last forever.
If you’re overwhelmed by the flood of questions, you might be wondering, “What’s next?” and “How do I manage my Parkinson’s?” This article will guide you through three crucial steps: learning about Parkinson’s Disease, establishing healthy habits, and building a supportive team. By following these steps, you’ll be better equipped to manage your condition and continue enjoying the activities you love.

1. Learn About Parkinson’s Disease
I am a firm believer that knowledge is power when it comes to Parkinson’s Disease. That is why I feel so strongly that everyone who has been diagnosed or those who have a close friend or family member with Parkinson’s Disease should take some time to learn about Parkinson’s Disease. Here’s how to start:
- Consult Reputable Sources: There’s a lot of information out there, so it’s crucial to rely on trusted sources like the Parkinson’s Foundation and the American Parkinson’s Disease Association. Don’t feel pressured to absorb everything at once; use these resources as ongoing references throughout your journey.
- Subscribe to Informative Newsletters: Join the MovementX Parkinson’s email list by filling out the form below. By joining this list you’ll get 1-2 emails each month with digestible amounts of information discussing various Parkinson’s Disease topics from traveling with Parkinson’s Disease to fall prevention tips. You can even request topics that interest you!
2. Establish Healthy Habits
Creating and maintaining healthy habits is crucial, though it’s easier said than done. Let’s break it down into manageable steps to help you make lasting changes.
Tips and Tricks
- Set Small, Achievable Goals: Break larger goals into smaller, manageable steps. For instance, if you haven’t been exercising regularly, start with a smaller goal of exercising 1-2 times a week and gradually increase. Small successes build momentum and make it easier to stick with new habits.
- Create a Routine and Stick to It: Make your new habits part of your daily schedule, just like you would a doctor’s appointment. Use calendars, alarms, or sticky notes to reinforce your routine and make it more attainable.
- Find Support and Accountability: Exercise is often more enjoyable with family or friends. Find someone who shares your interests and can support and encourage you.
- Engage in Activities You Enjoy: Focus on activities you love. If weightlifting isn’t your thing, try gardening or hiking. Enjoyable activities are easier to stick with and have a greater impact on your well-being.
- Ask for help: If you’re unsure where to start, don’t hesitate to ask for assistance! Later in this article, you’ll find a list of team members who can support you. If you need help finding the right professionals, feel free to reach out to me. I’d be happy to help connect you.
Habits to Monitor
- Exercise: Exercise is arguably one of the most effective treatment strategies for Parkinson’s Disease helping to manage an array of symptoms including balance, mobility, mood, and sleep to name a few. Aim for moderate to vigorous exercise for 30 minutes, 5 days a week but be sure to set small realistic goals for your as mentioned above. Programs like Rock Steady Boxing and Pedaling for Parkinson’s can be excellent starting points. Stay tuned for more information on this in future articles.
- Diet: Maintain a balanced diet to support overall health and manage symptoms. Again, little changes go a long way. Swap sugary drinks for water or opt for fresh fruit rather than a bag of chips. For a more individualized plan consult with a dietician.
- Medication: Keeping track of your medication is crucial. Use a pillbox to organize your meds and set recurring alarms on your phone or watch to remind you when to take them. Medication reminder apps can also be helpful.
- Mental Health: Parkinson’s Disease can affect your mood and emotional well-being. Engage in activities that promote relaxation and joy, and seek support from mental health professionals if needed. Regularly assess how you’re feeling and don’t hesitate to reach out for help if you notice changes in your mood or mental health.
- Sleep: Sleep issues are common in Parkinson’s Disease and can worsen symptoms. Establish a consistent sleep routine, create a comfortable sleep environment, limit screen time before bed, and address any sleep issues with your healthcare provider. Quality sleep is vital for managing symptoms and improving overall quality of life.
3. Build Your Team
Building a strong support team is essential for managing Parkinson’s Disease effectively. Here’s a rundown of key team members:
Physician
It’s crucial to have a neurologist experienced in Parkinson’s Disease or a Movement Disorder Specialist.
As Dr. Elizabeth Ferluga, Director of Movement Disorders at Synapticure, explains,
“A neurologist is a physician who has completed postgraduate training in neurology. A Movement Disorder Specialist is a neurologist who has gone a step further and completed a movement disorder fellowship. These subspecialists have extensive knowledge of movement disorders, particularly Parkinson’s Disease, and are knowledgeable about advanced treatment techniques, including deep brain stimulation, in addition to medication management.
Even early in Parkinson’s Disease, it is helpful to meet with a Movement Disorder Specialist to help create a holistic plan. Movement Disorder Specialists can either be your primary doctor or collaborate with your local neurologist to manage your condition. Due to high demand, you might need to travel long distances to see one.
However, at Synapticure, we offer virtual appointments with our Movement Disorder Specialists to improve access to care across the country. Our team also includes care coordinators, case managers, psychologists, genetic counselors, and speech therapists to provide comprehensive support.”
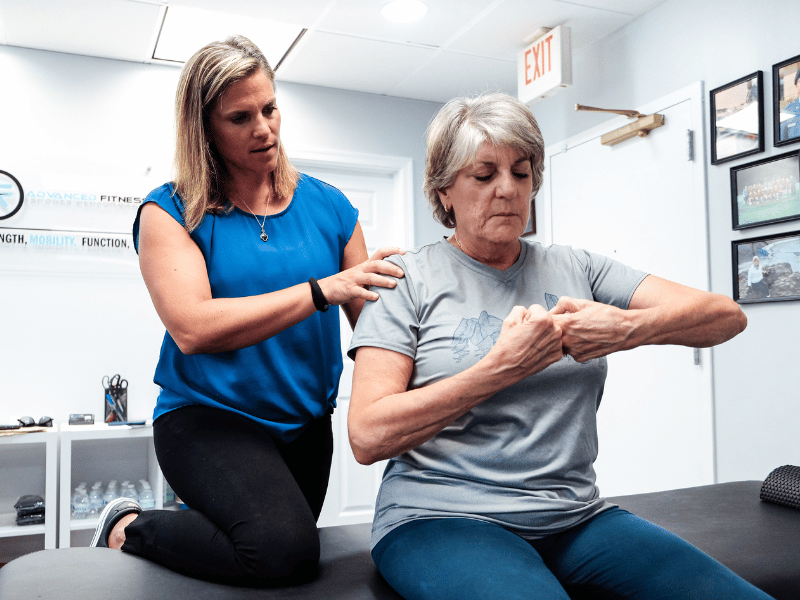
Physical Therapist
Physical therapy is crucial for improving and maintaining mobility, allowing you to continue enjoying the activities you love.
A key component of physical therapy is Core Set Testing, which provides objective data on mobility tasks such as walking speed, endurance, balance, and functional strength. After the test, your therapist will provide scores that assess your fall risk and track changes over time, helping to address issues early if needed. This data, combined with your personal goals, can guide effective treatment and exercise programs for better management of Parkinson’s Disease.
It’s important to work with a neurologic physical therapist who specializes in Parkinson’s Disease. If you need assistance finding an expert near you, feel free to contact me at lauren.scott@movement-x.com.
Occupational Therapist
Occupational therapy helps individuals with Parkinson’s Disease maintain independence and improve daily functioning and can recommend adaptive tools and techniques for tasks like dressing, cooking, and managing household chores. Additionally, OT can address fine motor skills and cognitive strategies to support overall daily performance.
Speech Therapist
Speech therapy is essential for managing communication and swallowing difficulties associated with Parkinson’s Disease. Speech therapists can help improve vocal strength, clarity, and articulation through specialized exercises and techniques. They also address swallowing issues, providing strategies to make eating and drinking safer and more comfortable.
Mental Health
Managing your mental health is a key part of dealing with Parkinson’s Disease, as the emotional toll can be significant. Mental health professionals can help address feelings of depression and anxiety, offering therapy and, if needed, medication to keep your emotional well-being in check.
Mental health professionals can also teach you stress-reduction techniques like mindfulness and provide strategies to build resilience. Remember, taking care of your mental health is just as important as managing your physical symptoms.
Support Team
Joining a support group for individuals with Parkinson’s Disease can provide valuable social connections and emotional support. Sharing experiences with others who understand your situation can reduce feelings of isolation and provide practical advice. Rock Steady Boxing is a great way to meet others who have Parkinson’s while working to maintain your physical mobility through guided exercise designed for people with Parkinson’s. Check out their website here: Rock Steady Boxing.

Conclusion
Being newly diagnosed with Parkinson’s Disease can feel overwhelming, but taking these steps can help you regain a sense of control. Remember, learning about your condition, establishing healthy habits, and building a supportive team are all critical parts of managing your health and well-being.
Have you thought about what steps you’ll take next? Are there specific areas where you feel you need more support or information? Reach out to organizations, join support groups, or talk to your healthcare team to explore options.
If you’re interested in starting physical therapy or want to learn more, sign up to connect with a specialized physical therapist or access our patient resources. We’re here to support you every step of the way.
References
- Osborne JA, Botkin R, Colon-Semenza C, et al. Physical Therapist Management of Parkinson Disease: A Clinical Practice Guideline from the American Physical Therapy Association. Physical Therapy. 2021;102(4). doi:https://doi.org/10.1093/ptj/pzab302







