Despite advances in healthcare, millions of people still suffer from chronic low back pain every year. Even with a wide range of available treatments — from pain medications to imaging to injections — many individuals find themselves stuck in a frustrating cycle where their symptoms never truly resolve.
If you’ve been dealing with lingering back pain despite your best efforts, you’re not alone. In this article, I’ll break down the real reasons why low back pain often persists — and what a smarter, more effective path to lasting relief actually looks like.
The Common Pitfalls That Keep Low Back Pain Chronic
Most people don’t end up with chronic low back pain because they’re “broken”—they end up there because traditional management strategies often miss the bigger picture.
Here are some of the most common traps that keep people stuck:
- Over-reliance on passive treatments: Short-term relief without addressing root causes.
- Fear of movement (kinesiophobia): Protecting the back to a fault, leading to more weakness and stiffness.
- Over-emphasis on imaging findings: Being told an MRI “problem” is the sole source of pain when often it’s not.
- Ignoring functional movement and lifestyle factors: Lack of movement variability and fitness.
- Neglecting long-term strength and conditioning: Skipping the crucial rebuild phase after pain subsides.
A Smarter Approach: What Actually Works
Solving chronic low back pain requires a shift in mindset — away from chasing temporary relief and toward building a resilient, confident body through a comprehensive, movement-focused plan.

1. Movement-Based Analysis of Meaningful Activities
Pain often surfaces during real-world movements like walking, squatting, lifting, or running. A skilled movement assessment looks beyond static tests and analyzes how your body functions dynamically.
By identifying stiffness, compensations, and inefficiencies, we can address the real drivers of your pain — not just manage the symptoms. For example, stiffness in the ribcage or hips can often drive lower back pain, even in the absence of any discomfort in those areas!

2. Lifestyle Modifications to Break Up Repetitive Positions
No posture is perfect for long periods. Problems arise when we stay in any one position too long.
Simple strategies like micro-breaks, position changes, and dynamic workstations can dramatically reduce tissue stress and fatigue. Even the best ergonomic set-ups can make it difficult to maintain a static position, and our bodies thrive on movement!

3. Manual Therapy Opens the Door – Movement Keeps It Open
Manual therapy (joint mobilizations, soft tissue techniques) can be incredibly effective — not because they “fix” tissues, but because they help modulate the nervous system and create a short-term window of opportunity for better movement.
As a clinician with thousands of hours in advanced hands-on training, I’ve come to appreciate these techniques for what they really are: a powerful gateway. They calm sensitivity, restore mobility, and reduce protective tone — but they’re only the beginning.
It’s what you do afterwards that really matters.
Prescriptive exercise is what turns short-term relief into long-term change. It reinforces mobility gains, retrains efficient motor patterns, and promotes neuroplasticity — helping the brain and body relearn how to move with confidence.
This isn’t just my clinical opinion — it’s backed by strong evidence. Research continues to show that combining manual therapy with movement-based re-education leads to better outcomes than either approach alone.

4. Long-Term Strength & Conditioning for Resiliency
Real recovery isn’t just about eliminating pain — it’s about building a body that can handle more, not less. Once pain decreases and mobility improves, the real work begins: progressive strength and conditioning.
My approach centers around retraining the fundamental movement patterns we all rely on every day: hinge, squat, lunge, push, pull, and carry. Whether you’re lifting a laundry basket, carrying groceries, squatting down to play with your kids, or returning to recreational sport, these patterns form the foundation of safe, efficient, and pain-free movement.
Strengthening these movements builds durability, confidence, and neuromuscular control — especially when tailored to your body’s history and goals. We don’t chase perfection or isolate muscles for the sake of exercise. We build functional strength that holds up under real-world stress.
And here’s the bonus: this style of movement training doesn’t just prevent re-injury — it often improves sports performance and helps break through frustrating fitness plateaus. When your body moves better, it performs better.
Research continues to show that well-designed strength training reduces the risk of future low back pain episodes and improves overall function better than passive care alone.
What About MRI Findings? The Truth About Imaging and Low Back Pain
It’s easy to be discouraged by MRI findings like “disc bulges” or “degenerative changes”, but here’s what many people aren’t told:
These findings are incredibly common — even in people with no pain at all.
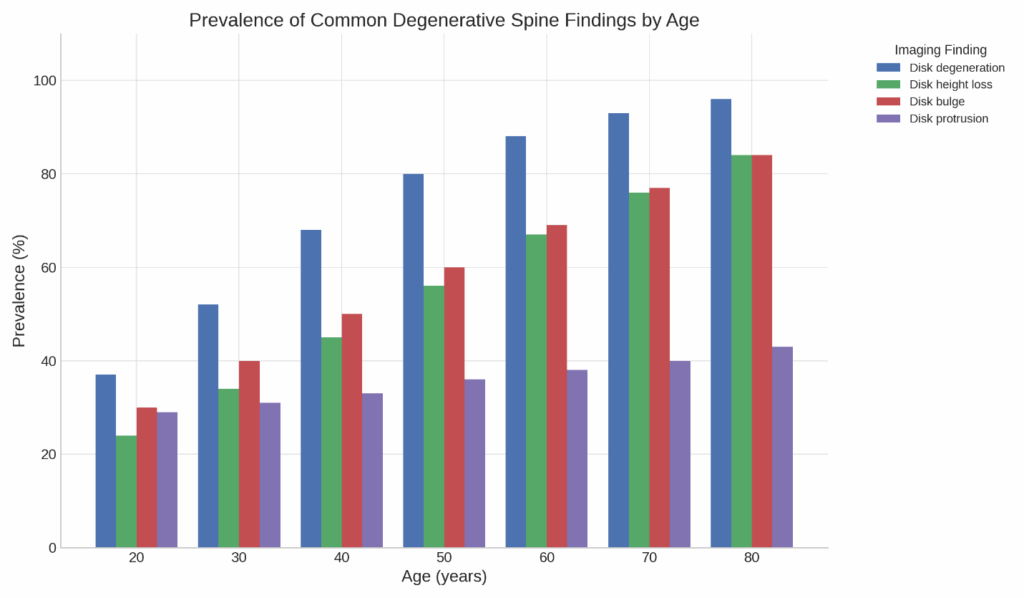
Spinal imaging findings are surprisingly common — even in people without back pain.
This chart shows how degenerative changes like disc bulges, disc height loss, and protrusions become more common as we age, even when no symptoms are present.
This is why treatment should focus on your movement, strength, and overall function — not just MRI results.
Abnormalities on imaging are often a normal part of aging (like wrinkles or gray hair) and should always be interpreted in the context of your symptoms and movement.
The Missing Link: Pain Science Education for Chronic Low Back Pain
One of the most misunderstood aspects of chronic low back pain is this:
pain doesn’t always mean actual tissue damage.
Even after tissue healing has occurred, pain can linger due to how the nervous system processes and responds to threat. Stress, fear, past experiences, beliefs, and even poor sleep can all influence how much pain you feel, regardless of what’s actually happening at the tissue level.
This is why it’s possible to still hurt even when your MRI looks unchanged… or why some days feel worse even when nothing “new” happened.
At its core, pain is a protective signal and can occur with actual or perceived tissue damage.
Understanding this is powerful. It reduces fear, helps you move more confidently, and puts you back in the driver’s seat.
Managing Low Back Pain Over a Lifetime
Even with great rehab, it’s normal for back pain to occasionally resurface.
But real success isn’t about eliminating every ache forever — it’s about knowing how to respond when it shows up.
Recovery becomes resiliency when you:
- Build physical tolerance through strength and movement
- Maintain smart habits that reduce flare-ups before they start
- Manage lifestyle drivers like stress, sleep, and recovery
- Understand how the brain and nervous system influence pain
When you have the right tools and you know how to use them, pain loses its power. You stop bracing for the worst… and start responding with confidence.
My goal for every patient isn’t just relief but to provide knowledge, strength, and strategies to stay in control for the long haul.
This is the difference between hoping it won’t come back… and knowing you can handle it if it does.
FAQ
Can chronic low back pain really get better without surgery?
Yes. Most chronic low back pain improves with conservative care focused on movement, strength, and education.
How long does it take to recover from chronic low back pain?
While timelines vary, meaningful improvement often occurs within 6–12 weeks of focused rehab addressing movement and strength.
If my MRI shows a disc bulge or degeneration, should I be worried?
No! Many people without any pain have disc changes on MRI. Function matters more than imaging. If you do have a relevant MRI finding, conservative care can often get you back to prior function without surgical intervention.
Is it normal for my back to hurt even after starting exercise?
Some discomfort is normal as the body adapts. Movement isn’t harmful when guided properly.
What’s the role of the brain in chronic pain?
The brain processes pain signals and can amplify or calm them. Pain neuroscience education helps retrain these systems.
Why do my hips and mid-back matter when my low back hurts?
Non-painful restrictions or weakness elsewhere can place stress on the lower back. Identifying and addressing regional influences provides better long-term outcomes than local treatment alone. If you’d like to learn how different regions of the body connect to influence recovery, check out my previous blog post on regional interdependence here.
References
- Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., … & Kallmes, D. F. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American Journal of Neuroradiology, 36(4), 811-816. https://doi.org/10.3174/ajnr.A4173
- Fritz, J. M., Cleland, J. A., & Brennan, G. P. (2007). Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Medical Care, 45(10), 973–980. https://doi.org/10.1097/MLR.0b013e318070c6cd
- Louw, A., Diener, I., Butler, D. S., & Puentedura, E. J. (2016). The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of Physical Medicine and Rehabilitation, 97(10), 1720–1733. https://doi.org/10.1016/j.apmr.2016.03.004
- Maher, C., Underwood, M., & Buchbinder, R. (2017). Non-specific low back pain. The Lancet, 389(10070), 736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
- Moseley, G. L. (2003). Joining forces–combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. The Journal of Manual & Manipulative Therapy, 11(2), 88-94. https://doi.org/10.1179/106698103790826378
- O’Sullivan, P. (2012). It’s time for change with the management of non-specific chronic low back pain. British Journal of Sports Medicine, 46(4), 224–227. https://doi.org/10.1136/bjsm.2010.081638
- Puentedura, E. J., & Louw, A. (2012). A neuroscience approach to managing athletes with low back pain. Physical Therapy in Sport, 13(3), 123–133. https://doi.org/10.1016/j.ptsp.2011.06.001
- Steele, J., Bruce-Low, S., Smith, D., Jessop, D., Osborne, N., & Narici, M. (2021). A review of the effectiveness of resistance training for back pain. Sports Medicine, 51(6), 1103–1122. https://doi.org/10.1007/s40279-020-01396-w
About the Author
Dr. Adam Kays is a physical therapist and Board-Certified Orthopedic Clinical Specialist in Central Indiana. Among Adam’s treatment specialities are spine disorders, headaches, trigeminal neuralgia, and dry needling. Dr. Adam believes in empowering his patients through education and exercise self-efficacy to help you return to your favorite fitness activities better than before.








